By Sherrie Dulworth
Originially Published: January 2018
Despite changes that may loom on health care’s horizon, many experts agree that value-based payments are here for the foreseeable future. Along with government Medicare and Medicaid initiatives, Forbes reported that almost half of the payments from the nation’s largest insurers are now built on a value-based formula.
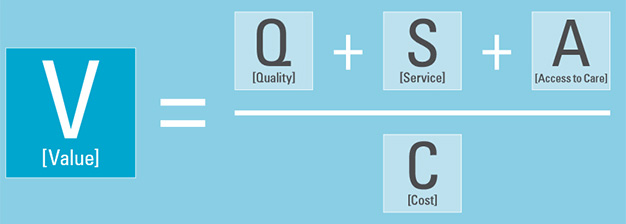
Value-based payment (VBP) models typically shift from paying providers for encounters (activity) to paying for care based on a hybrid formula of quality, service, access and cost.
In the past 24 months, The HealthSearch Group has seen a growing interest and awareness among our clients of how VBP agreements will influence their organizational recruiting, retention and training.
We spoke with three health care thought-leaders who shared their value-based purchasing insights and expertise.
Rethinking the Status Quo
These arrangements can create opportunities for innovation; however, success is not guaranteed. “There’s going to be winners and losers,” said Chuck Bongiovanni, a consultant who helps provider organizations prepare for success under new payment models.
Prospering under VBP requires that organizations rethink the status quo, including the broad areas of talent acquisition, training and deployment.
Bongiovanni used an example of finance and case management, historically disparate areas, one broadly focused on cash and the other clinical, with employees who were not necessarily well-versed in the other area.
Financial losses to an organization have implications for everyone and cross-training can help yield insights and opportunities for improvement. “There needs to be a marriage of perspectives and knowledge,” Bongiovanni said.
What talent is needed to succeed under VBP contracts, where are the talent gaps, and how best to fill those?
A Value Project Report by the Healthcare Financial Management Association describes ways to prepare for optimized VBP performance. Provider organizations anticipate talent investments in certain key services including information technology, data analytics, clinical care coordination and patient experience/engagement.
It’s more than a potential increase in head-count alone as the nuances of the required expertise or expectations may vary from a fee-for-service, or even capitated, environment.
For instance, part of the value-based equation is increased efficiency in when, where, and how clinical care is delivered. This means eliminating or reducing delays that often lead to poor clinical outcomes. That may seem intuitive, but it has implications for employee recruiting and expectations. For example, coordinating patient assessments and care delivery within best practice timeframes requires the ability to deploy resources, throughout all care settings, on a seven-day-a-week basis. It’s not enough to have enough people but also imperative to have the right people doing the right things.
Provider organizations are also seeking solid network management and contracting expertise, both strategic and tactical know-how, for services that span across episodes of care.
According to Patricia Richards, “there is a nexus where the use of meaningful data, care management, quality, finance and contracting all come together.”
Richards, the Director, CMS Innovations & Value-Based Programs at New Brunswick’s Saint Peter’s Healthcare System, explained that population health expertise, with a view of quality and cost across the continuum of care, can help achieve business and clinical transformation.
According to Brett Friedman, a partner with a healthcare practice group at the law firm Ropes & Gray LLP, organizational compliance infrastructure may have more complex needs and systems requirements as a result of VBP.
VBP incentivizes providers to transition from volume-based reimbursement methodologies to alternative forms of payment that may reward providers for better health outcomes.
“Providers are now far more connected with others in the health care system through accountable care organizations and other entities that are designed to achieve clinical integration among different types of community-based organizations,” said Friedman. “Those relationships may include data sharing agreements and innovative contracting models that reward these affiliates for behavior that contributes to overall care improvements, as measured based on the data being collected.”
Friedman added that conducting solid monitoring and auditing of these new payment models may require broader expertise and training within compliance departments that utilize complementary skill-sets.

Another growing area of talent need among provider organizations is data analytics, but under VBP, professionals may need proficiency to mine and analyze not only encounter data but claims data, traditionally an information resource within the insurance realm.
Human Resources and VBP
VBP represents a paradigm change in service delivery for many organizations and predictably, both a challenge and opportunity. With VBP, like all areas of health care, the human resources of an organization are a vital investment and an important variable in the equation for success.